Crohn’s Disease: Everything You Need To Know

Crohn’s disease is a chronic inflammatory disease of the walls of the gastrointestinal tract, usually the intestine. Associated symptoms mainly include diarrhea, abdominal pain and fever.
Inflammatory bowel disease
Inflammatory bowel diseases (in English inflammatory bowel diseases – IBD ) are characterized by chronic inflammation of the intestinal walls for unspecified causes with a chronic relapsing course. This category includes ulcerative colitis and Crohn’s disease.
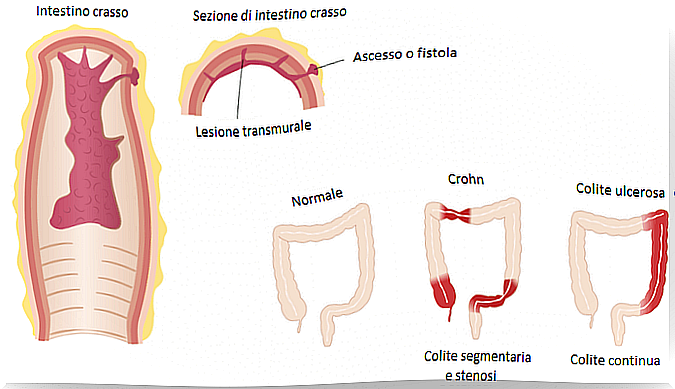
Ulcerative colitis affects only the mucous membrane of the colon walls, while Crohn’s disease affects the entire intestinal wall and any intestinal segment, although generally in a segmental and asymmetrical manner.
The causes of Crohn’s disease are not known with certainty, but the most widespread theory is that of multifactorial pathogenesis : in other words, Crohn’s disease could be the consequence of a series of genetic, environmental, microbiological and immunological factors.
Symptoms of Crohn’s Disease
- Diarrhea, usually bloody
- Abdominal pain
- Abdominal mass
- Weight loss
- Fatigue
- Rectal tenesmus
- Temperature
Crohn’s disease can lead to complications such as:
- Abscesses
- Fistulas
- Intestinal obstruction
- Stenosis
- Perianal disease
- Toxic megacolon
A relationship has been found between Crohn’s disease and an increased predisposition to develop colon cancer. However, scholars have not come to more specific conclusions given the lack of certain etiology regarding the pathology itself.
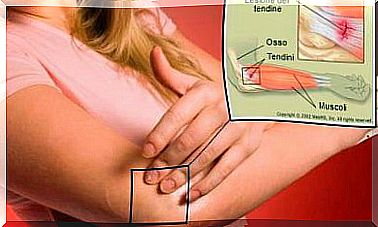
Extraintestinal manifestations
In relation to the degree of activity:
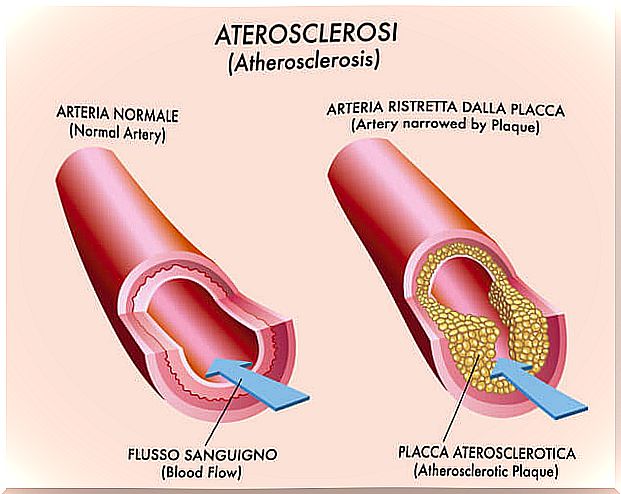
- Peripheral arterial disease
- Erythema nodosum
- Epiescleritis
- Aphthous stomatitis
- Fat liver
Independent of the degree of activity:
- Gangrenous pyoderma
- Psoriasis
- Ankylosing spondylitis
- Uveitis and sacroiliitis
Crohn’s Disease Diagnosis
The diagnosis of inflammatory bowel disease requires clinical data, laboratory and histological analyzes, as well as endoscopic and radiological tests. There is no specific test to detect the disease.
Celiac enteropathy and intestinal infections must be ruled out because both involve inflammation of the mucous membrane.
The lack of a specific analysis for the detection of inflammatory bowel disease leads to a slowdown in the diagnosis process.
Endoscopy
Endoscopy is used for the initial and differential diagnosis to determine the extent and severity of the lesions, as well as the presence or absence of neoplasia, to evaluate the response to treatment and in some cases it is also used as a therapeutic method.
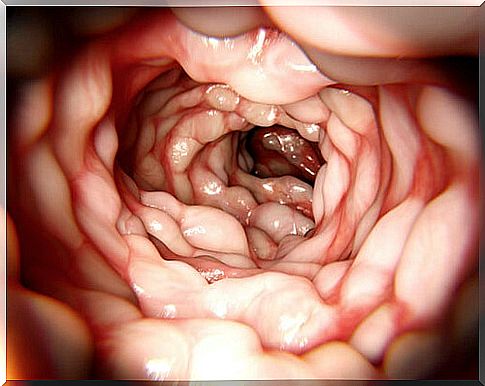
Ileocolonoscopy is the procedure used during the initial evaluation of Crohn’s disease.
Radiology
Several radiological studies are carried out, including those involving the use of contrast media, ultrasound, CT and magnetic resonance imaging. Radiological studies help identify edema, ulcers, strictures, fistulas and extraintestinal manifestations.
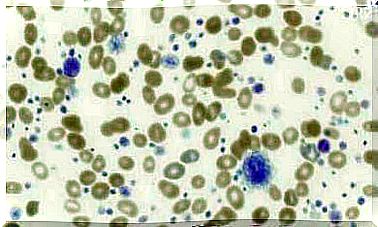
Histology
Biopsy in Crohn’s disease is a very important test for the differential diagnosis with other possible pathologies. The main pathological features of Crohn’s disease are:
- Continuous distribution of lesions affecting the intestinal wall
- Presence of granulomas
- Presence of lymphocytes and plasma cells
- Irregularity of the intestinal glands or crypts
Laboratory analysis
Calprotectin testing determines the presence of intestinal inflammation based on the amount of this protein in the stool.
In addition, the patient undergoes general analyzes to assess his health condition.
Crohn’s disease classification
Patients are classified according to the age at which the disease appears, the location of the disease and the pattern of the disease itself, according to the Montreal Classification.
- Age
- A1: under 16 years old
- A2: from 16 to 40 years
- A3: from 40 years old
- Location
- L1: Ileus
- L2: Colon
- L3: Ileus and colon
- L4: when the disease affects the upper digestive tract
- Type of disease
- B1: inflammatory type
- B2: stenosing type
- B3: fistulizing type
- P: when the disease affects the perianal area.
Crohn’s disease activity index
The Harvey activity index allows to recognize the stage of the disease according to some clinical criteria.
The patient’s general well-being, abdominal pain, the number of liquid depositions throughout the day, or the frequency of diarrhea, and the presence of abdominal masses or any complications are assessed.
The total index score can indicate disease remission, moderate or marked activity. Based on this, the severity of the disease and its treatment can be established.